Case description
A 42-year-old female with no significant medical history or prior abdominal surgery presented with a sudden onset of severe abdominal pain, lasting five hours before the admission. In the previous months, she experienced similar pain with spontaneous remission. The patient suffered from nausea, but had no stool irregularities or vomiting. Urinary symptoms or signs of infection were not documented.
Clinical examination depicted a patient in decreased general condition with significant abdominal pain. There was pronounced tenderness in the right upper quadrant of the abdomen and left and right lumbar region. There were no signs of peritonitis. Laboratory analysis revealed leukocytosis 12.39 x 10^9/L, normal CRP 1 mg/L, hyponatremia 135 mmol/L, hypokalemia 3.1 mmol/L, and lactate 3.29 mmol/L. Liver, pancreatic and renal tests were within normal limits, pregnancy test was negative and there was a microhematuria without signs of urinal infection.
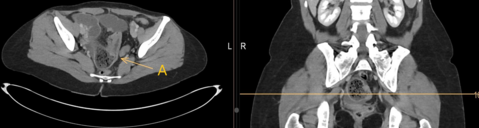
An abdominal computed tomography (CT) with intravenous contrast showed the following images:
What is the most likely diagnosis?
- Volvulus
- Foramen of Winslow hernia
- Hiatus hernia
- Adhesion ileus
Pertaining to the previous answer, what would be the preferable course of treatment?
- Prokinetic therapy
- Immediate laparoscopy
- Immediate laparotomy
- Observation and follow-up CT scan/elective operation
Case solution
The abdominal CT revealed a mechanical ileus. The cecum and a part of the ascending colon were herniated through foramen of Winslow into the bursa omentalis, being strangulated and massively distended. (Fig.1a,1b) The correct answer to the first question is B.
Internal hernias account for 1% of all abdominal hernias, and only about 8% of them involve herniation through the foramen of Winslow (1). In the literature, cecal or ascending colon herniation is the second most prevalent type, comprising 30% of cases, followed by small bowel herniation at 67% (1,2). Risk factors include a mobile cecum, an intraperitoneal ascending colon, a long mesentery, or a dilated foramen of Winslow (3). Surgical intervention remains unanimously the treatment for internal hernias. However, due to a limited sample size and diverse local findings, there is no universally accepted standard of care. Since the introduction of laparoscopic management in 2011 by van Daele et al. (4), there has been a growing recommendation to approach each foramen Winslow hernia laparoscopically, even if bowel resection is warranted (5). Some surgeons opt for hernia reduction only ( 5,6), while cases of ischemia may necessitate resection and anastomosis (5,7). Even in cases with a viable colon, systematic right hemicolectomy is recommended when an adequate peritonisation cannot be achieved (8, 9, 10).
The correct answer to the second question is thus, once more B. The laparoscopic repositioning of the hernia and revision of the small bowel proved to be impossible. We decided to convert to laparotomy for better access and assessment. Upon ventral opening of the bursa omentalis, the incarcerated bowel segment, with visible tenia coli and a non-inflamed appendix, was identified as the cecum and part of the ascending colon. (Fig.2a) Manual reduction of the hernia revealed a hypermobile cecum with a lack of posterior attachment, indicative of malrotation. (Fig.2b) A right hemicolectomy with a side-to-side isoperistaltic anastomosis was performed to remove the damaged cecum and prevent recurrent hernias. The patient was discharged three days postoperatively without complications. At the one-month follow-up, the patient was doing well and reported no symptoms or difficulties.
- Evrard V, Vielle G, Buyck A, Merchez M. Herniation through the foramen of Winslow. Report of two cases. Dis Colon Rectum. 1996 Sep;39(9):1055-7.
- Osvaldt AB, Mossmann DF, Bersch VP, Rohde L. Intestinal obstruction caused by a foramen of Winslow hernia. Am J Surg. 2008 Aug;196(2):242-4.
- Makra GM, Dechantsreiter G, Holzapfel K. Innere Hernierung des Zökums durch das Foramen epiploicum (Winslowi) in die Bursa omentalis. Rofo. 2019 Jan;191(1):67-69.
- Van Daele E, Poortmans M, Vierendeels T, Potvlieghe P, Rots W. Herniation through the foramen of Winslow: a laparoscopic approach. Hernia. 2011 Aug;15(4):447-9.
- Duinhouwer LE, Deerenberg E, Rociu E, Kortekaas RT. Herniation of the colon through the foramen of Winslow-A case report. Int J Surg Case Rep. 2016;24:14-7.
- Daher R, Montana L, Abdullah J, d'Alessandro A, Chouillard E. Laparoscopic management of foramen of Winslow incarcerated hernia. Surg Case Rep. 2016 Dec;2(1):9.
- Makarawo T, Macedo FI, Jacobs MJ. Cecal bascule herniation into the lesser sac. World J Clin Cases. 2014 Dec 16;2(12):903-6.
- Forbes SS, Stephen WJ. Herniation through the foramen of Winslow: radiographic and intraoperative findings. Can J Surg. 2006 Oct;49(5):362-3.
- Samson TD, Tercero FM, Sato K, Awad ZT, Filipi CJ. Cecal herniation through the foramen of Winslow after laparoscopic Nissen fundoplication. Surg Endosc. 2001 Dec;15(12):1490.
- Azar AR, Abraham C, Coulier B, Broze B. Ileocecal herniation through the foramen of Winslow: MDCT diagnosis. Abdom Imaging. 2010 Oct;35(5):574-7.