Case description:
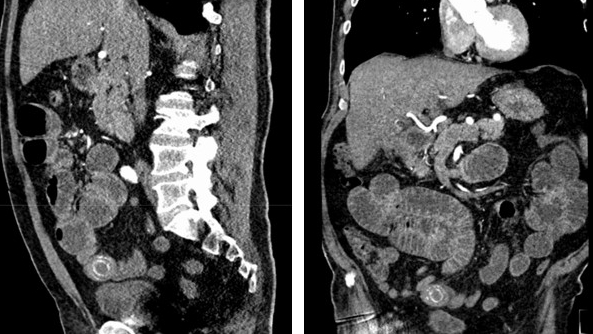
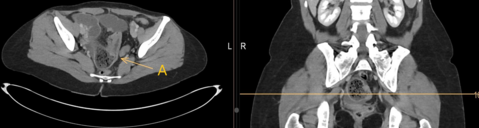
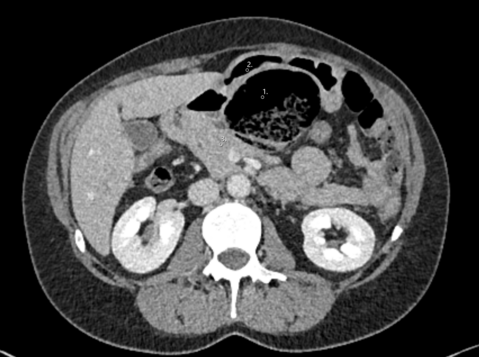
A 70-year-old male patient presented to the emergency department in mild distress, with a 4-day history of intermittent, diffuse abdominal pain, vomiting, and nausea of increasing frequency. The patient reported three similar episodes of abdominal pain and constipation over the past year, successfully managed with dietary modifications. Previous colonoscopies showed a lymphoproliferative malignancy at 30 cm as well as a few benign polyps removed via endoscopy. Physical examination revealed mild cutaneous jaundice, hyperactive bowel sounds, and abdominal tenderness in the right and left lower abdominal quadrants. The vital signs showed tachycardia and hypotension as well as an elevated respiratory rate. Blood work revealed a slightly elevated CRP of 21 mg/l, marked leucocytosis due to a history of chronic lymphocytic leukaemia (CLL), evidence of acute-on-chronic renal insufficiency, as well as mild hyperbilirubinemia. Blood gas analysis showed metabolic alkalosis with normal lactate levels. The patient was not on any regular medication. After stabilising the patient and initiating fluid resuscitation, a CT scan was performed, revealing:
What is the most appropriate course of action in this patient?
A. Fluid resuscitation, nasogastric tube, treatment with laxatives
B. Diagnostic laparoscopy/laparotomy due to suspicion of mechanical bowel obstruction
C. Laparoscopic cholecystectomy due to suspicion of acute cholecystitis
D. Fluid resuscitation, followed by endoscopy and renewed biopsy
E. Fluid resuscitation followed by chemotherapy due to CLL progress
Case solution:
The correct answer is B
The patient was prepped for surgery for suspicion of gallstone ileus. The stone was removed via longitudinal enterotomy. Gallstone ileus is a rare cause of mechanical bowel obstruction, caused by the entry of a gallstone via biliary-enteric fistula (1,2). It has been postulated that persistent pericholecystic inflammation results in adhesions between the gallbladder and enteric system. This in turn may lead to pressure necrosis, erosion, and formation of biliary-enteric fistula (3). Gallstones exceeding 2cm may impact, especially in the ileum (4,5). Patients generally present with a” tumbling obstruction “, i.e., recurrent obstruction and abdominal pain as the stone works its way through the digestive tract (5). The mainstay of treatment remains surgical intervention and enterolithotomy. In patients considered ¨high risk¨, such as advanced age, comorbidities, severe upper right quadrant inflammation, and dense fibrous adhesions, an enterolithotomy, with or without bowel resection to relieve intestinal obstruction may be sufficient. Thereafter, an expectant management can be pursued as biliary-enteric fistulas may shrink or even close if the cystic duct is patent. (1,6). Should the patient have recurrent symptoms, elective cholecystectomy may be warranted (6). In low-risk patients, fit individual with a concomitant need for biliary surgery at the time of presentation, a single operation involving enterolithotomy, cholecystectomy, and biliary-enteric fistula revision is attempted (5,7). These options must be weighed against the reported rates of recurrence of 8.3% (1).
- Halabi WJ, Kang CY, Ketana N, et al. Surgery for gallstone ileus: a nationwide comparison of trends and outcomes. Ann Surg 2014; 259:329.
- van Hillo M, van der Vliet JA, Wiggers T, et al. Gallstone obstruction of the intestine: an analysis of ten patients and a review of the literature. Surgery 1987; 101:273.
- Beltran MA, Csendes A, Cruces KS. The relationship of Mirizzi syndrome and cholecystoenteric fistula: validation of a modified classification. World J Surg 2008; 32:2237.
- Deitz DM, Standage BA, Pinson CW, et al. Improving the outcome in gallstone ileus. Am J Surg 1986; 151:572.
- Clavien PA, Richon J, Burgan S, Rohner A. Gallstone ileus. Br J Surg 1990; 77:737.
- Reisner RM, Cohen JR. Gallstone ileus: a review of 1001 reported cases. Am Surg 1994; 60:441.
- Ayantunde AA, Agrawal A. Gallstone ileus: diagnosis and management. World J Surg. 2007; 31:1292-7