Case description:
An 80-year-old male patient presented to the emergency department in moderate distress with a one-day history of dull, pressing pain in the lower right abdomen with no nausea or vomiting. The pain developed four days after an unremarkable colonoscopy. His medical history included metabolic syndrome, Barrett's esophagus, duodenal adenomas, coronary artery disease, atrial fibrillation, and an open appendectomy at the age of 20 years. Current medications were a proton pump inhibitor, a statin, metformin, amlodipine, and aspirin.
On physical examination, the patient appeared mildly ill. The abdomen was soft but tender in the lower right quadrant with mild distension and no rebound tenderness.
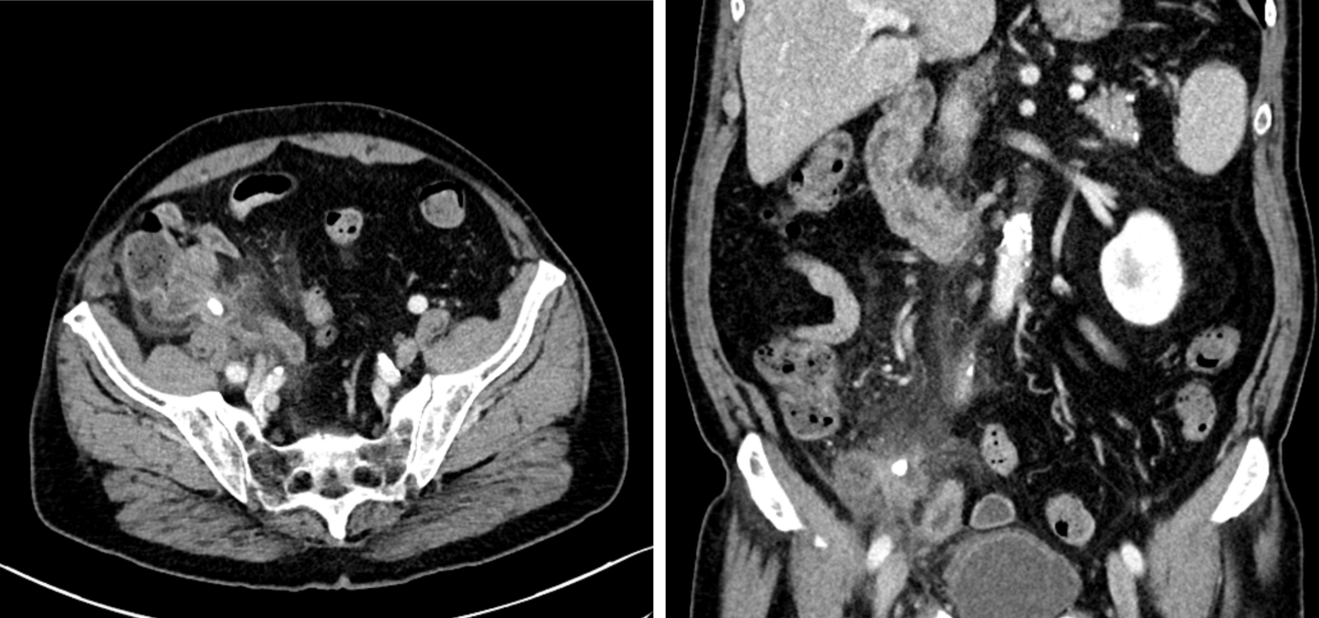
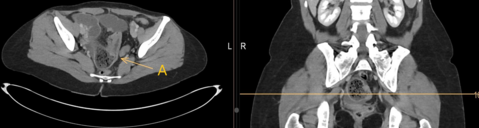
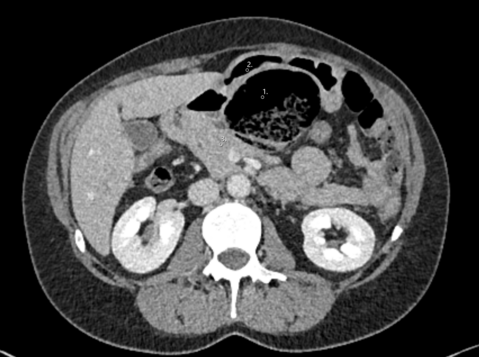
Vital signs were as follows: blood pressure of 152/73 mmHg, heart rate of 81 bpm, SpO2 of 95%, and an initial temperature of 37.1°C, rising to 38.5°C three hours after presentation. Blood work revealed mild leukocytosis (10.8 thousand/ml), thrombocytopenia (138 thousand/ml), and an elevated C-reactive protein (CRP) of 97 mg/l (reference range <5 mg/l). After considering possible differential diagnoses, a computed tomography scan with intravenous contrast was performed, revealing:
Question: What is the most likely diagnosis and most appropriate course of action?
A. Adhesive small bowel obstruction. Laparoscopic adhesiolysis
B. Gallstone ileus. Laparoscopic enterolithotomy
C. Ureterolithiasis. Analgesia and urologic consult
D. Stump appendicitis. Laparoscopic stump appendectomy
E. Uncomplicated diverticulitis. Antibiotic treatment
Case Solution:
The correct answer is D
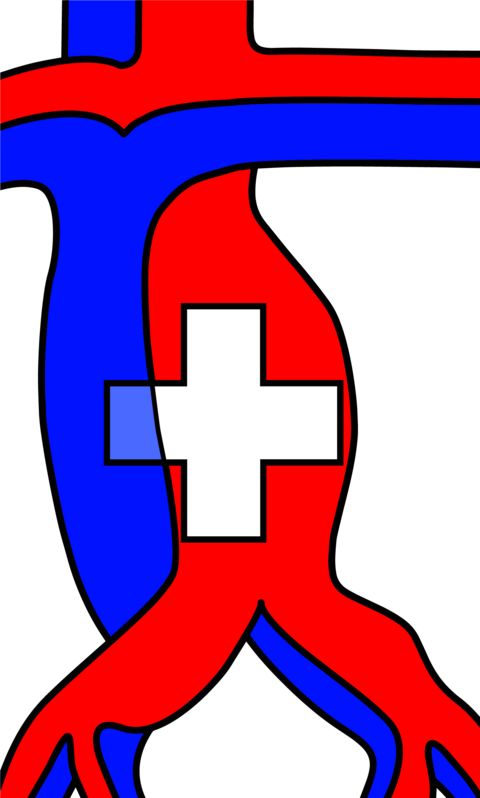
The CT scan (Figure A) showed an inflamed, fluid-filled structure at the ileocecal junction containing an 8 mm calcified stone, accompanied by fat stranding. The patient was prepped for surgery for suspicion of stump appendicitis (SA), a rare postoperative complication of appendectomy that involves inflammation of residual appendiceal tissue (1). During laparoscopic appendectomy, the appendiceal stump was visualized and was found to have a perforation (Figure B). The appendicolith was extracted, and the residual appendix was resected using a 60 mm stapler. The patient was discharged on the second postoperative day with stable vital signs and regular bowel and bladder function. Follow-up blood work at the primary care physician’s office on the fourth postoperative day revealed declining CRP (29 mg/l) and leukocyte count (5.5 thousand/ml).
SA is a late complication but can occur at any time after appendectomy; independent of the surgical approach used in the original procedure (2). SA poses a diagnostic challenge because clinicians often rule out appendicitis in patients with a history of appendectomy (3). Delay in treatment can lead to complications similar to those seen in appendicitis, including perforation, periappendiceal abscess, and sepsis (4). Malignancy of the appendiceal stump has also been reported (5). In a review conducted by Casas et al. (1), 76 SA cases were analyzed, showing a higher prevalence in male and younger patients (mean 36.6 years) with a median time interval between initial appendectomy and SA of 5.2 months. Our patient represents a rarer case of SA, being the oldest patient and having the longest SA interval described in the literature (1,2). This case underscores the importance of considering SA as a differential diagnosis and promptly utilizing proper imaging such as ultrasound or CT in any patient presenting with abdominal pain characteristic of acute appendicitis and a history of appendectomy.
- Casas MA, Dreifuss NH, Schlottmann F. High-volume center analysis and systematic review of stump appendicitis: solving the pending issue. Eur J Trauma Emerg Surg. 2022 Jun;48(3):1663–72.
- Kanona H, Al Samaraee A, Nice C, Bhattacharya V. Stump appendicitis: a review. Int J Surg. 2012;10(9):425–428.
- Yuksel Y, Ergun T, Torun E, Ozen O. Recurrent stump appendicitis. Am J Emerg Med. 2021 Jun;44:481.e3-481.e5.
- Johnston J, Myers DT, Williams TR. Stump appendicitis: surgical background, CT appearance, and imaging mimics. Emerg Radiol. 2015 Feb;22(1):13–8.
- Al-Tarakji M, Muhammad Ali S, Khalaf M, Shahid F, Mohamed SSI. Adenocarcinoma of Stump Appendicitis: An Extremely Rare Pathology - A Literature Review. Cureus. 2020 Jul 30;12(7):e9482.